*Use of loop diuretics should be limited to the management of patients with volume
overload and not for AKI or oliguria per se.
* It is not necessary to wait until severe uremia develops to initiate dialytic support; renal
replacement therapy should be used as a supportive therapy in the presence of progressive
azotemia and oliguria, rather than a rescue therapy for late manifestation of AKI.
*It is well established that individuals with CKD have a 10- to 20-fold increased risk for
cardiac death compared to age-matched and gender-matched controls without CKD.
*The weight loss drug orlistat rarely may cause acute kidney injury and nephrolithiasis
because its use may lead to intestinal malabsorption and enteric hyperoxaluria.
*. The antiseizure and migraine drug topiramate is a carbonic anhydrase inhibitor that is
associated with proximal renal tubular acidosis and calcium phosphate stone formation.
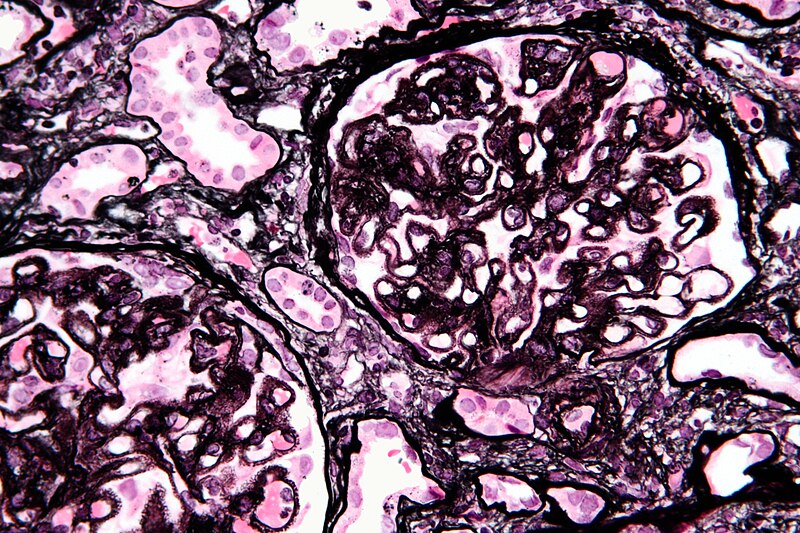
*The natural history of the primary nephrotic syndrome depends on the underlying cause.
Thus, patients with minimal change nephrotic syndrome (MCNS) have an excellent
long-term prognosis, in contrast to those with primary focal segmental glomerulosclerosis
(FSGS), in whom nearly 50% will progress to end-stage renal disease (ESRD) over 5 to
10 years of follow-up, and 25% to 30% of these patients may experience recurrent
disease in a kidney transplant.

overload and not for AKI or oliguria per se.
* It is not necessary to wait until severe uremia develops to initiate dialytic support; renal
replacement therapy should be used as a supportive therapy in the presence of progressive
azotemia and oliguria, rather than a rescue therapy for late manifestation of AKI.
*It is well established that individuals with CKD have a 10- to 20-fold increased risk for
cardiac death compared to age-matched and gender-matched controls without CKD.
*The weight loss drug orlistat rarely may cause acute kidney injury and nephrolithiasis
because its use may lead to intestinal malabsorption and enteric hyperoxaluria.
*. The antiseizure and migraine drug topiramate is a carbonic anhydrase inhibitor that is
associated with proximal renal tubular acidosis and calcium phosphate stone formation.
*The natural history of the primary nephrotic syndrome depends on the underlying cause.
Thus, patients with minimal change nephrotic syndrome (MCNS) have an excellent
long-term prognosis, in contrast to those with primary focal segmental glomerulosclerosis
(FSGS), in whom nearly 50% will progress to end-stage renal disease (ESRD) over 5 to
10 years of follow-up, and 25% to 30% of these patients may experience recurrent
disease in a kidney transplant.