Now these patients usually need renal replacement therapy. Whenever we consider Peritoneal dialysis in these patients, we must consider patients ventriculo-peritoneal shunt which is often placed in these pateint because of Hydrocephalous. Therefor these children would be prone to meningitis if PD is initiated.
Tuesday, 31 July 2012
Spina Bifida(Neurogenic bladder.)
Now these patients usually need renal replacement therapy. Whenever we consider Peritoneal dialysis in these patients, we must consider patients ventriculo-peritoneal shunt which is often placed in these pateint because of Hydrocephalous. Therefor these children would be prone to meningitis if PD is initiated.
Monday, 23 July 2012
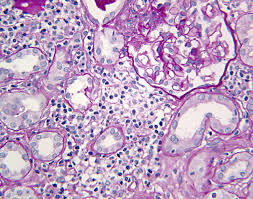
Interstitial nephritis
How interstitial nephritis is presented and what are the some of the drugs which cause?
It is usually presented with fever. maculopapular rash, eosinophilia, eosinophilurea.
Penicillin analogue, cephalosporin, sulphonamide, NSAIDs, cimitidine, allopurinol etc.
It is usually presented with fever. maculopapular rash, eosinophilia, eosinophilurea.
Penicillin analogue, cephalosporin, sulphonamide, NSAIDs, cimitidine, allopurinol etc.
Monday, 7 May 2012
Question solution
- A 30 year female of Chronic nephritis/CRF had a live related renal transplant 1 year back. She seeks your advice regarding future pregnancy. She is receiving Prednisolone, Cellcept and cyclosporine as maintenance immunosuppression . Her BP is well controlled with Enalpril 5mg once daily.
a) How
would u assess her suitability of successful outline of pregnancy what advice
would you give?
b) What
if any modification in her current medication is required should she become
pregnant?
c) What complications are expected?
Answere: Assessment of suitability regarding
pregnancy and advice entails:
Assessment of her current renal
function, her urine detail report and her course post transplant sofar.
At least 1 year post‐transplantation
Stable renal function with creatinine
<2 mg/dl
No recent episodes of acute
rejection
BP ≤140/90 mmHg on medications
Proteinuria <500 mg/day
Prednisone ≤15 mg/day Azathioprine
≤2 mg/kg/day
Cyclosporin ≤4 mg/kg/day
Normal allograft ultrasound
b) Replace cellcept with
azathioprin and enalpril with methyldopa. Atenolol and metoprolol can also be
given. In severe hypertension nefidipine and hydralazine can be given.
d) Gestational
diabetes, preeclamsia, preterm labour .
Rate of uti more especially whose primarily
renal disease is secondary to Pyelonephritis.
Friday, 20 April 2012
Nephrotic syndrom
What are the diagnostic criteria for nephrotic syndrome?
Nephrotic syndrome is a syndrome that results from severe proteinuria. Heavy glomerular
protein losses (3.5 g in an adult or .40 mg/m2/hour in a child) lead to the other three
criteria for nephrotic syndrome: hypoalbuminemia, hyperlipidemia, and usually edema.
From a practical standpoint, measuring a urine total protein/creatinine ratio is preferable
to collecting a 24-hour urine for protein. A ratio of 3.5 correlates with nephrotic-range
proteinuria.
2. What is minimal change disease (minimal change nephrotic syndrome)?
Minimal change disease (MCD) is a disorder of glomeruli that leads to heavy proteinuria.
Renal biopsy shows normal glomeruli by light microscopy but will show effacement of the
podocyte foot processes by electron microscopy. Immunofluorescent microscopy typically
is negative, although some patients may show staining for immunoglobulin M (IgM) in the
mesangial regions of the glomeruli. Technically, a patient cannot be said to have MCD with
certainty without having had a kidney biopsy. However, so many young children with
nephrotic syndrome have MCD that kidney biopsies are only performed in those children
with atypical findings or in those who are resistant to immunosuppressive therapy. Older
adolescents and adults are diagnosed with MCD after a kidney biopsy is performed.
3. How likely is MCD to be the cause of nephrotic syndrome in any individual?
MCD is the cause of nephrotic syndrome in about 90% of children younger than age 6, in
about 65% of older children, and in about 20% to 30% of adolescents. In adults only about
10% to 25% of nephrotic syndrome results from MCD, but it represents the third most
common cause of nephrotic syndrome in adults after membranous nephropathy and focal,
segmental glomerulosclerosis.
4. What causes MCD?
MCD is an immune-mediated disease, felt to be mediated by a circulating factor capable of
inducing proteinuria. Presumably the circulating factor is secreted by lymphoid cells, and it
functions as a vascular permeability factor that directly affects the function of the podocytes.
Although the majority of cases of MCD are idiopathic, MCD, particularly in adults, may be
associated with neoplastic disease such as lymphoma, toxic or allergic reactions to drugs,
certain infections, allergies, or other autoimmune disorders.
5. How common is MCD?
The prevalence of MCD in children is about 16 per 100,000 children, but it is much less
prevalent in adults.
6. What is the typical clinical presentation of MCD?
Patients with MCD typically present with mild to severe edema. Because the onset with
periorbital edema commonly follows an upper respiratory infection in young children,
nephrotic syndrome may sometimes be confused with an allergic reaction until a more
thorough evaluation is performed. I
Nephrotic syndrome is a syndrome that results from severe proteinuria. Heavy glomerular
protein losses (3.5 g in an adult or .40 mg/m2/hour in a child) lead to the other three
criteria for nephrotic syndrome: hypoalbuminemia, hyperlipidemia, and usually edema.
From a practical standpoint, measuring a urine total protein/creatinine ratio is preferable
to collecting a 24-hour urine for protein. A ratio of 3.5 correlates with nephrotic-range
proteinuria.
2. What is minimal change disease (minimal change nephrotic syndrome)?
Minimal change disease (MCD) is a disorder of glomeruli that leads to heavy proteinuria.
Renal biopsy shows normal glomeruli by light microscopy but will show effacement of the
podocyte foot processes by electron microscopy. Immunofluorescent microscopy typically
is negative, although some patients may show staining for immunoglobulin M (IgM) in the
mesangial regions of the glomeruli. Technically, a patient cannot be said to have MCD with
certainty without having had a kidney biopsy. However, so many young children with
nephrotic syndrome have MCD that kidney biopsies are only performed in those children
with atypical findings or in those who are resistant to immunosuppressive therapy. Older
adolescents and adults are diagnosed with MCD after a kidney biopsy is performed.
3. How likely is MCD to be the cause of nephrotic syndrome in any individual?
MCD is the cause of nephrotic syndrome in about 90% of children younger than age 6, in
about 65% of older children, and in about 20% to 30% of adolescents. In adults only about
10% to 25% of nephrotic syndrome results from MCD, but it represents the third most
common cause of nephrotic syndrome in adults after membranous nephropathy and focal,
segmental glomerulosclerosis.
4. What causes MCD?
MCD is an immune-mediated disease, felt to be mediated by a circulating factor capable of
inducing proteinuria. Presumably the circulating factor is secreted by lymphoid cells, and it
functions as a vascular permeability factor that directly affects the function of the podocytes.
Although the majority of cases of MCD are idiopathic, MCD, particularly in adults, may be
associated with neoplastic disease such as lymphoma, toxic or allergic reactions to drugs,
certain infections, allergies, or other autoimmune disorders.
5. How common is MCD?
The prevalence of MCD in children is about 16 per 100,000 children, but it is much less
prevalent in adults.
6. What is the typical clinical presentation of MCD?
Patients with MCD typically present with mild to severe edema. Because the onset with
periorbital edema commonly follows an upper respiratory infection in young children,
nephrotic syndrome may sometimes be confused with an allergic reaction until a more
thorough evaluation is performed. I
Thursday, 19 April 2012
Acid Base Disorder
Question 1
The primary disturbance in this patient is an acidosis, as indicated by the acidemic pH in the blood (pH 7.0). The normal bicarbonate concentration is 24 mmol/L but this patient’s bicarbonate concentration is 8 mmol/L. This indicates a fall in bicarbonate of 16 mmol/L.
Thus, there is a primary metabolic acidosis.
The anion gap is 22.
Recall, anion gap is calculated by the formula:
AG = Na – HCO3 – Cl
AG = 140 – 8 – 110
AG = 22
The normal anion gap is about 12, so the anion gap is increased.
Thus, there is an anion gap metabolic acidosis.
The anion gap is increased by 10 but the bicarbonate has fallen by 16mmol/L. Therefore, there is also a fall in bicarbonate that is not accounted for by the H+ ions that accompanied the unmeasured anions in this case – this means there is also a non-anion gap metabolic acidosis.
The bicarbonate has decreased by 16.
We would expect that in a metabolic acidosis, there would be a 1 mmHg fall in pCO2 for every 1 mmol/L of bicarbonate.
Therefore, we would expect that the pCO2 would be 24 mmHg. Since it is 35mmHg, it is too high and this represents a respiratory acidosis.
Describe the acid-base diagnosis in the following case (for example, metabolic acidosis with compensatoryrespiratory alkalosis):
A 41 year old male presents to the ER with the following lab results (hint: look for multiple simultaneous problems).
Na 140 mmol/L
K 4.0 mmol/L
Cl 110 mmol/L
pH 7.0
pCO2 35 mmHg
pO2 75 mmHg
HCO3 8 mmol/L
Answer:A 41 year old male presents to the ER with the following lab results (hint: look for multiple simultaneous problems).
Na 140 mmol/L
K 4.0 mmol/L
Cl 110 mmol/L
pH 7.0
pCO2 35 mmHg
pO2 75 mmHg
HCO3 8 mmol/L
The primary disturbance in this patient is an acidosis, as indicated by the acidemic pH in the blood (pH 7.0). The normal bicarbonate concentration is 24 mmol/L but this patient’s bicarbonate concentration is 8 mmol/L. This indicates a fall in bicarbonate of 16 mmol/L.
Thus, there is a primary metabolic acidosis.
The anion gap is 22.
Recall, anion gap is calculated by the formula:
AG = Na – HCO3 – Cl
AG = 140 – 8 – 110
AG = 22
The normal anion gap is about 12, so the anion gap is increased.
Thus, there is an anion gap metabolic acidosis.
The anion gap is increased by 10 but the bicarbonate has fallen by 16mmol/L. Therefore, there is also a fall in bicarbonate that is not accounted for by the H+ ions that accompanied the unmeasured anions in this case – this means there is also a non-anion gap metabolic acidosis.
The bicarbonate has decreased by 16.
We would expect that in a metabolic acidosis, there would be a 1 mmHg fall in pCO2 for every 1 mmol/L of bicarbonate.
Therefore, we would expect that the pCO2 would be 24 mmHg. Since it is 35mmHg, it is too high and this represents a respiratory acidosis.
Therefore, this is a case of a
- Anion gap metabolic acidosis
- Non-anion gap metabolic acidosis
- Respiratory acidosis
Subscribe to:
Comments (Atom)